Acute renal impairment in stroke patients; an Upper Egypt clinical, laboratory and radiological study
Gharib Fawi Mohamed1, Ali Taha2, Mohammed Abdallah Abbas3, Hassan Mohammed1, Al-Amir Bassiouny Yossef1
1Department of neuropsychiatry, Sohag University.
2Department of internal medicine, Sohag University.
3Department of neuropsychiatry, South Valley University.
Abstract
Background: acute renal impairment is a common complication after acute stroke. More than one fourth of patients developed acute kidney injury in the first 2 days after the ictus.
Aim of the work: To study the prevalence of acute renal impairment in acute stroke patients and to study the clinical characteristics, risk factors, laboratory and radiological findings of stroke patients with and without acute kidney injury.
Subjects and Methods: The study included 500 patients admitted to the Neurology department of Sohag university hospital, Alhelal hospital and Sohag general hospital presented by stroke within the first 48 hours. Patients with a history of renal disease or receiving dialysis for chronic renal failure were excluded. Patients were subjected to detailed medical and neurological evaluation. Stroke severity assessed by NIHSS, Glasgow coma scale and MRCS of power. CT brain was done for all patients and laboratory studies were done including serum urea, creatinine, calculated creatinine clearance, uric acid, electrolyte assessment, random blood sugar, liver functions test, coagulation profile, complete blood count and erythrocyte sedimentation rate.
Results: Renal impairment was reported in 122 patients (24.4%). The mean age “mean ± SD” of patients without AKI was 61.61±12.977 and that of patients with AKI was 64.71±10.653. In patients without AKI, the percentage of male was 52.1% and in patients with AKI, male percentage was 56.5%. In patients without AKI, we reported the following; hypertension (25.1%), ACEIs (44%), atrial fibrillation (10.8%), coma (2.8%), DM (36.5%), hyperlipidemia (34.1%), smoking (29.6%), cardiac disease (31.4%), hyperuricemia (14%), TIA (1.8%), drug abuse (3.1%), mean Na level (139.6±6.6), mean K+ (4.2±1.6), mean Ca++ (9.1±.5), echogenic grade (I) kidney on U/S (7.4%), cerebral infarction (68%), cerebral hemorrhage (31%) and hemorrhagic infarction (0.7%). In patients with AKI, we reported the following; hypertension (19.6%), ACEIs (55%), atrial fibrillation (11.4%), coma (5.4%), DM (36.8%), hyperlipidemia (30.3%), smoking (23.7%), cardiac disease (26.2%), hyperuricemia (25%), TIA (1.6%), drug abuse (7.3%), mean Na level (134.9±6.3), mean K+ (4.2±.9), mean Ca++ (8.5±.8), echogenic grade (I) kidney on U/S (59.1%), cerebral infarction (56.5%) and cerebral hemorrhage (41%).
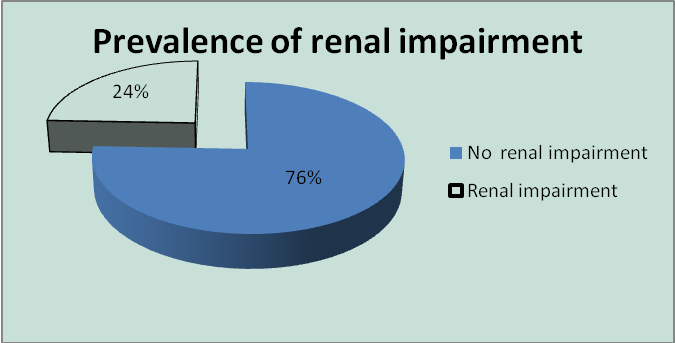
Conclusion: we found that the prevalence of renal impairment in acute stroke patients is 24.4% and its predictors were age, conscious level, presence of speech abnormality, hypertension, hyperuricemia, RHD, drug abuse, presence of casts, crystals and albumin in urine, elevated ALT enzyme, leucocytosis and high ESR.
INTRODUCTION
Stroke, after cardiovascular disease and cancer, is the third cause of death in developed countries1,2. Generally acute renal failure (ARF) is defined as an abrupt and sustained decline in renal function, which results in disturbances in electrolyte and acid-base homeostasis, derangement in extracellular fluid volume and retention of nitrogenous waste products. ARF develops in about 5% of all hospitalized patients and in 5-25% of patients admitted to ICUs, and the highest incidence, approximately 50%, has been reported in patients with septic shock3-8. It was found that acute kidney injury (AKI) is a common complication after acute stroke. More than one fourth (27%) of patients developed AKI in the first 2 days after the ictus9.
AIM OF THE WORK
To study the prevalence of acute renal impairment in acute stroke patients and to study the clinical characteristics, risk factors, laboratory and radiological findings of stroke patients with and without acute kidney injury.
PATIENTS AND METHODS
The study was done on 500 patients admitted to the Neurology department of Sohag university hospital, Alhelal hospital and Sohag general hospital presented by stroke within the first 48 hours. Diagnosis of stroke was confirmed by CT. Patients with no confirmed CT brain or those suspected of having transient ischemic attack (TIA) were excluded from the study. Also patients with a history of renal disease or receiving dialysis for chronic renal failure were excluded.
Patients were subjected to:
Detailed medical and neurological evaluation, with special stress on the following parameters:
Age, gender, history of hypertension, diabetes mellitus, hypercholesterolemia, hyperuricemia, past history of TIA or ischemic stroke, presence of ischemic heart disease or cardioembolic disease, atrial fibrillation (AF), previous and current antiplatelet treatment, current alcohol overuse, smoking or substance abuse. Pulse rate (PR), regularity, arterial blood pressure on admission and every 6 hours after admission. Systolic and diastolic hypertension is considered when systolic blood pressure ≥140mmHg and diastolic blood pressure ≥90 respectively. Diabetes mellitus was diagnosed based on history of fasting blood glucose levels >126 mg/dL and/or the use of anti-diabetic agents.
Definition of acute kidney injury (AKI): All patients with a rise in serum creatinine value or fall in GFR (as per RIFLE, whichever was greater) were included in the AKI group and were assigned to a category in the RIFLE classification10.
Determination of the stroke severity on admission according to: NIHSS, Glasgow coma scale and MRCS of power.
Computerized tomography (CT) brain.
Ischemic stroke: To confirm the diagnosis of stroke and to determine the distribution of stroke and presence of leucoariosis
Hemorrhagic stroke: Topographic classification of the hematoma will be assessed as the following: hematomas that predominantly affected the subcortical white matter of the cerebral lobes will be defined as lobar, while those in the basal ganglia, thalamus, or both will be defined as deep. The presence of intraventricular blood associated with bleeding outside the ventricles is considered to represent intraventricular spread of the hematoma. Mass effect will be defined as the presence of midline shift displacement by ≥ 5 mm on brain CT.
Other neuroimaging investigations if need: MRI, CT angiography for SAH
Laboratory studies:
Serum urea, creatinine, calculated creatinine clearance (ml/min), was calculated by use of a recent version of the Cockcroft-Gault equation as follows:
(140-age) X 1.26 X weight (kg) X k/ plasma creatinine (µmol), where; k=1 if male or 0.85 if female11,12.
Uric acid, electrolyte assessment; Na+, K+, Ca++, random blood sugar, liver functions test, coagulation profile, complete blood count (CBC) and erythrocyte sedimentation rate (ESR).
Statistical analysis
Analysis of data was carried out using the "Statistical Program for Social Sciences" (SPSS) for windows version 19.0. Categorical variables were expressed as frequency and percentage while continuous variables were expressed as mean±standard deviation. Pearson Chi-square and independent student’s (t) test were used in univariate analysis. P value < 0.05 was used as a significance level.
RESULTS
Demographic data
The study was carried on 500 patients, 266 males (53.2 %) and 234 females (46.8%), presented with stroke within the first 48 hours of onset. The mean age of patients (Mean +SD) is 62.37±12.5.
Prevalence of renal impairment
Renal impairment (creatinine 1200 µm) was reported in 122 patients (24.4%).
Fig (1) Prevalence of renal impairment in stroke patients
Demographic data in both groups (without AKI and with AKI)
The mean age “mean ± SD” of patients without AKI was 61.61±12.977 and that of patients with AKI was 64.71±10.653 (P-value=0.017). In patients without AKI, the percentage of male was 52.1% while female percentage was 47.8% and in patients with AKI, male percentage was 56.5%, while female percentage was 43.4%, (P-value = 0.3).
Clinical characteristics and risk factors of both groups of patients (table 1):
Hypertension was reported in 25.1% of patients without AKI versus 19.6% of patients with AKI (P-value=0.218). The mean±SD of SBP/DBP in patients without AKI was 156.9±30.3/90.4±11.7 versus 165.66±33.7/96.1±18 in patients with AKI (P-value= 0.007). The most common type of treatment was ACEIs (44%) in patients without AKI versus 55% in patients with AKI (P-value= 0.000). AF was the most common type of cardiac arrhythmia reported in patients without and with AKI (10.8% and 11.4% respectively) (P-value= 0.000). Coma (GCS<8) was reported in 2.8% of patient without AKI and in 5.4% of patient with AKI (P-value=0.000). The most common type of speech abnormality in patient with and without AKI was dysarthria (39% and 6.4% respectively) (P-value=0.000). Right hemiplegia was reported in 43.1% and 59% of patient without and with AKI respectively while left hemiplegia was reported in 40.7% and 32.7% (P-value= 0.001). Fits were reported in 5% of total patients, most of them were focal fits (3.4%), while generalized tonic clonic fits was reported in 1.6% of patients (P-value= 0.000).
The total percentage of DM among stroke patients was 36.6% and about 36.5% reported in patients without AKI versus 36.8% reported in patients with AKI (P-value=0.940). IDDM was reported in 19.8% of patients without AKI versus 25.4% in patients with AKI (P-value=0.227) while NIDDM reported in 16.6% in patients without AKI versus 11.4% in patients with AKI (P-value=0.22). Mean RBS was 190.8±(105.1) of patients without AKI versus 220.8±(127.6) in patients with AKI (P-value= 0.010). Hyperlipidemia was reported in 34.1% of patients without AKI versus 30.3% in patients with AKI (P-value=0.438). Smoking was reported in 29.6% of patients without AKI versus 23.7% in patients with AKI (P-value=0.211). Cardiac disease was reported in 31.4% of patients without AKI versus 26.2% in patients with AKI (P-value=0.288). Hyperuricemia was reported in 14% of patients without AKI versus 25% in patients with AKI (P-value=0.003). Mean uric acid was 5.2±2 of patients without AKI versus 6.4± 4.3 in patients with AKI with statistically significant difference between both groups (P-value= 0.000). TIA was reported in 1.8% of patients without AKI versus 1.6% in patients with AKI (P-value=0.878). Dysarthria was the most prevalent speech deficit and reported in 1.5% of patients without AKI versus 1.6% of patients with AKI (P-value=0.850). Previous stroke was reported in 10.8% of patients without AKI versus 14.7% in patients with AKI (P-value=0.236). Right hemiplegia was the most prevalent motor deficit and reported in 6.6% of patients without AKI versus 9% of patients with AKI (P-value= 0.618). Drug abuse was reported in 3.1% of patients without AKI versus 7.3% in patients with AKI (P-value= 0.044). Opium was the most common abused substance and reported in 1.8% of patients without AKI versus 5.7% in patients with AKI (P-value= 0.07).
Table 1: Clinical characteristics and risk factors of both groups of patients:
|
P value |
With AKI |
Without AKI |
Clinical data |
P value |
With AKI |
Without AKI |
Clinical data |
|
|
33(27 %) |
103( 27.2%) |
IHD |
|
|
|
HTN |
|
|
|
|
MI/cardiac |
0.218 |
24( 19.6%) |
95(25.1%) |
Not hypertensive |
|
0.932 |
118(96.7 %) |
365(96.5 %) |
No MI |
|
98( 80.3%) |
283( 74.8%) |
Hypertensive |
|
|
4( 3.2%) |
13( 3.5%) |
MI |
0.007 |
165.66± 33.7 |
156.90±30.3 |
SBP |
|
|
|
|
Duration |
|
96.15± (18) |
90.40±11.7 |
DBP |
|
|
93(76.2 %) |
279(73.8 %) |
Non MI |
|
|
|
Duration |
|
0.425 |
0(0 %) |
8( 2.1%) |
First discovered |
|
24( 19.6%) |
95(25.1%) |
Non hypertensive |
|
|
11( 9%) |
34(8.9 %) |
< 2 years |
0.173 |
45( 36.8%) |
106 (28 %) |
First discovered |
|
|
15( 12.2%) |
40(10.5 %) |
2-5 years |
|
9(7.3 %) |
50(13.2 %) |
< 2 years |
|
|
3(2.4 %) |
17( 4.4%) |
> 5 |
|
25(20 %) |
61(16.1 %) |
2-5 years |
|
|
|
|
CCU admission |
|
19( 15.5%) |
66(17.4 %) |
> 5 years |
|
|
120(98.3 %) |
367(97 %) |
No CCU |
|
|
|
Treatment |
|
0.443 |
2( 1.6%) |
11 ( 3%) |
CCU/MI |
|
24( 19.6%) |
95(25.1%) |
Not hypertensive |
|
|
|
|
RHD |
0.238 |
67( 55%) |
166(44 %) |
ACEIs |
|
0.031 |
122(100 %) |
364(96.2 %) |
No RHD |
|
14( 11.4%) |
50(13.2 %) |
B blockers |
|
|
0 |
14(3.7 %) |
RHD |
|
12(9.8 %) |
37(9.7 %) |
Ca channel blockers |
|
|
|
|
Open HS |
|
0 |
9(2.3 %) |
Diuretics |
|
0.077 |
120(98.3 %) |
378(100 %) |
No |
|
|
|
Pulse |
|
|
1(0.8 %) |
0 |
Yes |
0.178 |
82.92±(6.8) |
81.91±(7.2) |
Mean |
|
|
|
|
Uric acid |
0.490 |
100( 82%) |
317(83.8 %) |
Regular |
|
0.003 |
91(75 %) |
325(86 %) |
Normal |
|
22( 18%) |
61(16.1%) |
Irregular |
|
0.000 |
31(25 %) 6.4± 4.3 |
53( 14%) 5.2± 2.0 |
Hyperuricemia |
|
|
|
Type of irregularity |
|
|
|
|
TIA |
0.885 |
14( 11.4%) |
41(10.8%) |
AF |
|
0.878 |
120(98.3%) |
371(98%) |
No TIA |
|
8(6.5 %) |
20(5.2%) |
Ventricular ectopic |
|
|
2( 1.6%) |
7( 1.8%) |
TIA |
|
|
|
DM |
|
|
|
|
Deficit |
0.940 |
77( 63.1%) |
240( 63.4%) |
Non diabetic |
|
|
120(98.3 %) |
371(98.1 %) |
Normal |
|
45( 36.8%) |
138(36.5 %) |
Diabetic |
|
0.850 |
2(1.6 %) |
6(1.5 %) |
Dysarthria |
|
|
|
Duration |
|
|
0(0%) |
1(0.2 %) |
Left hemiplegia |
|
77( 63.4%) |
240( 63.1%) |
Non diabetic |
|
|
|
|
Duration before stroke |
0.319 |
11( 9%) |
49(12.9%) |
First discovered |
|
|
120(98.3 %) |
371(98.1%) |
Normal |
|
7( 5%) |
29(7.6 %) |
< 2 years |
|
0.842 |
2( 1.6%) |
7( 1.8%) |
< 2 years |
|
16( 13%) |
28( 7.4%) |
2-5 years |
|
|
0 |
1( 0.2%) |
2-5 years |
|
11(9 %) |
32(8.4 %) |
> 5 years |
|
|
|
|
Treatment |
|
|
|
Type |
|
|
120(98.3 %) |
371(98.1%) |
Normal |
|
77( 63.4%) |
240( 63.1%) |
Not diabetic |
|
0.750 |
2(1.6 %) |
4(1 %) |
No ttt |
0.227 |
14(11.4 %) |
63(16.6 %) |
NIDDM |
|
|
0 |
1(0.2 %) |
Antiplatelet |
|
31( 25.4%) |
75( 19.8%) |
IDDM |
|
|
|
|
Previous stroke |
0.873 |
|
|
Regular /not on treatment |
|
0.236 |
104(85.2%) |
337(89.1%) |
No |
|
77( 63.4%) |
240( 63.1%) |
Not diabetic |
|
|
18( 14.7%) |
41( 10.8%) |
Yes |
|
39(31.9 %) |
115 (30.4%) |
Regular |
|
|
|
|
Deficit |
|
6(4.9 %) |
23( 6%) |
Not regular |
|
|
104(85.2%) |
337(89.1%) |
Normal |
0.010 |
220.8±(127.6) |
190.8±(105.1) |
Mean RBS |
|
0.618 |
2( 1.6%) |
4(1 %) |
Dysarthria |
|
|
|
Hyperlipidemia |
|
|
11(9 %) |
25(6.6%) |
Right hemiplegia |
0.438 |
85( 69.6%) |
249( 65.8%) |
No |
|
|
5(4 %) |
12(3.1 %) |
Left hemiplegia |
|
37( 30.3%) |
129( 34.1%) |
Yes |
|
|
|
|
Duration |
|
|
|
duration |
|
|
104(85.2%) |
337(89.1%) |
Normal |
0.388 |
85( 69.6%) |
249( 65.8%) |
No hyperlipedemia |
|
0.081 |
5( 4%) |
22(5.8%) |
< 2 years |
|
34( 27.8%) |
119( 31.4%) |
First discovered |
|
|
12(9.8 %) |
15(4 %) |
2-5 years |
|
1(0.8 %) |
6( 1.5%) |
< 2 years |
|
|
1(0.8 %) |
4(1 %) |
> 5 years |
|
1(0.8 %) |
4(1 %) |
2-5 years |
|
|
|
|
Treatment |
|
1(0.8 %) |
0 |
> 5 years |
|
|
104(85.2%) |
337(89.1%) |
Normal |
|
|
|
Smoking |
|
0.765 |
9(7.3%) |
22(5.8 %) |
No ttt |
0.211 |
93( 76.2%) |
266(70.3 %) |
Nonsmoker |
|
|
9( 7.3%) |
21(5.5 %) |
Antiplatelet |
|
29(23.7 %) |
112(29.6%) |
Smoker |
|
|
|
|
OCP |
|
|
|
SI |
|
|
68(55.7 %) |
198( 52.3%) |
Male |
|
93( 76.2%) |
266(70.3 %) |
Nonsmoker |
|
0.624 |
53(43.4 %) |
176( 46.5%) |
Non |
0.468 |
2( 1.6%) |
6( 1.5%) |
X smoker |
|
|
1( 0.8%) |
4( 1%) |
Yes |
|
2( 1.6%) |
13(3.4 %) |
Stop smoker |
|
|
|
|
Drug abuse |
|
13( 10.6%) |
36(9.5 %) |
Mild smoker |
|
0.044 |
113(92.6 %) |
366(96.8 %) |
No |
|
6( 4.9%) |
38(10 %) |
Moderate smoker |
|
|
9(7.3%) |
12( 3.1%) |
Yes |
|
6(4.9 %) |
19(5 %) |
Severe smoker |
|
|
|
|
Type/drug abuse |
|
|
|
Cardiac |
|
|
113(92.6 %) |
366(96.8 %) |
Non |
0.288 |
90(73.7 %) |
259(68.5 %) |
Not cardiac |
|
0.074 |
2(1.6 %) |
5(1.3 %) |
Cannabis |
|
32( 26.2%) |
119( 31.4%) |
Cardiac |
|
|
7( 5.7%) |
7( 1.8%) |
Opium |
|
|
|
IHD |
|
|
|
|
|
0.851 |
89(72.9 %) |
275(72.7 %) |
No IHD |
Laboratory findings
1-Prevalence of renal impairment: renal impairment (creatinine ≥1.2 mg) was reported in 24.4% of total number of patients.
2-Urine analysis: acidic PH was reported in 99.4% of patients without AKI versus 24.4% in patients with AKI (P-value=0.421). Casts was reported in 1.6% of patients without AKI versus 6.5% in patients with AKI (P-value= 0.004). Crystals was reported in 26.5% of patients without AKI versus 48.3% of patients with AKI (P-value= 0.000). Cox was the most prevalent crystal and reported in 3.1% of patients without AKI versus 5.7% of patients with AKI. Trace of albumin in urine was reported in 1% of patients without AKI versus 5.7% of patients with AKI (P-value= 0.002). Hematuria was more severe in patients without AKI with mean RBC’s in urine 3.82±5.9 versus 9.47±7.1 in patients with AKI (P-value= 0.000).
3-Electrolytes: the mean Na level was 139.6±6.6 in patients without AKI versus 134.9±6.3 in patients with AKI (P-value= 0.000). The mean K+ was 4.2±1.6 in patients without AKI versus 4.2±.9 in patients with AKI (P-value= 0.688). The mean Ca++ was 9.1±.5 in patients without AKI versus 8.5±.8 in patients with AKI (P-value= 0.000).
4-Liver enzymes: the mean AST was 32.30±38.8 in patients without AKI versus 39.49±43.3 in patients with AKI (P-value= 0.085). The mean ALT was 31.71±30.6 in patients without AKI versus 46.98±58.9 in patients with AKI (P-value= 0.000).
5-Coagulation profile: the mean prothrombin concentration was 92.9±12.2 in patients without AKI versus 21.5±1.9 in patients with AKI (P-value= 0.2).
6-Complete blood picture (CBC): the mean RBC's was 4.275±0.623 in patients without AKI versus 4.210±0.635 in patients with AKI (P-value= 0.321). The mean WBC's was 10.6±0.98 in patients without AKI versus 13.4±6.19 in patients with AKI (P-value= 0.000). The mean Platelets was 293.45±81.5 in patients without AKI versus 287.02±71.8 in patients with AKI (P-value= 0.436).
7-ESR: the mean 1st hr ESR was 12.826±0.6 in patients without AKI versus 27.20±18.4 in patients with AKI (P-value= 0.000). The mean 2nd hr ESR was 46.92±22.6 in patients without AKI versus 53.98±27.5 in patients with AKI (P-value= 0.005).
Radiological findings:
U/S kidney: Echogenic grade (I) kidney on U/S was reported in 7.4% of patients without AKI versus 59.1% in patients with AKI (P-value= 0.000).
U/S Liver: Enlarged liver and liver Cirrhosis was reported only in patients with AKI (1.6% and 0.8% respectively).
CT brain: Cerebral infarction was reported in 68% of patients without AKI versus 56.5% in patients with AKI while cerebral hemorrhage was reported in 31% of patients without AKI versus 41% in patients with AKI but hemorrhagic infarction was reported only in patients without AKI (0.7%). Multiplicity of cerebral infarction was reported in 9.7% of patients without AKI versus 7.3% in patients with AKI (P-value= 0.423).
Distribution of infarction: PACI was reported in 41% of patients without AKI versus 31.1% in patients with AKI, next lacunar infarction was reported in 16% of patients without AKI versus 5.7% in patients with AKI, then POC was reported in 6% of patients without AKI versus 5.7% in patients with AKI and finally TACI was reported in 5.5% of patients without AKI versus 14% in patients with AKI.
Intraventricular extension: IV was reported in 5.8% of patients without AKI versus 18.8% in patients with AKI (P-value= 0.000).
Site of ICH: The most prevalent site of cerebral hemorrhage was reported in basal ganglia (15% of patients without AKI versus 18% in patients with AKI) next parietal hemorrhage was reported in 12% of patients without AKI versus 17.2% in patients with AKI then brain stem was reported in 1% of patients without AKI versus 5% in patients with AKI then subarachnoid hemorrhage was reported only in of patients without AKI (1.5%) then intraventricular hemorrhage was reported in 0.8% of patients without AKI finally cerebellar hemorrhage was reported in 0.5% of patients without AKI versus 0.8% in patients with AKI.
Midline shift: ML shift was reported in 17% of patients without AKI versus 36.8% in patients with AKI (P-value= 0.000).
Hydrocephalus: Hydrocephalus was reported in 5.2% of patients without AKI versus 15.5% in patients with AKI (P-value= 0.000).
Leucoariosis: Leucoariosis was reported in 32.8% of patients without AKI versus 32% in patients with AKI (P-value= 0.997).
DISCUSSION
Our study was done on 500 patients presented with acute stroke within the first 48 hrs after onset and admitted to the Neurology department-Sohag University Hospital, Al-Helal Hospital and Sohag General Hospital.
Prevalence of renal impairment in stroke patients:
AKI is a common complication after acute stroke, more than one fourth of patients (26.7%) developed AKI in the first 2days after the ictus9. Reduced eGFR on admission reported in 26.3% of stroke patients13. Almost one-third (28.08%) of acute stroke patients presented with moderate or severe renal dysfunction9. A similar high proportion of patients who presented within 48h of ictus had renal dysfunction despite the differences in the risk profile of patients14. AKI is an independent prognostic factor for mortality after stroke and was present in 14.29% of stroke patients15. The prevalence of renal impairment (creatinine> 1.2 mg) in our series about 24.4%. Our findings not only reinforce the results of previous studies but also provide additional data on predictors of renal impairment. The reasons of differences in previous studies may be due to different baseline characteristics of participants, different methods to evaluate renal function and different classification of renal dysfunction.
Clinical characteristics and risk factors of both groups of patients:
Age and renal impairment: AKI developed more frequently in older persons, with a higher creatinine/lower GFR at baseline15-17. Our study found that renal impairment on admission more common in older than younger age.
Sex and renal impairment: AKI occurrence was strongly associated with male gender17. Our study found that renal impairment on admission in men was slightly more frequent than in women (13.8% versus 10.6% respectively).
Predictors of renal impairment in stroke patients:
The independent predictors of reduced eGFR were age, gender, hematocrit on admission, history of hypertension, history of diabetes, and NIHSS scores upon admission, among which hypertension and diabetes were modifiable factors13. Our study found that the predictors of renal impairment were age, conscious level, presence of speech abnormality, hypertension, hyperuricemia, RHD, drug abuse, presence of casts, crystals and albumin in urine analysis, elevated ALT enzyme, leucocytosis and high ESR With this issue is important and has a significant impact on short term outcome of stroke, but studies are lacking.
SUMMARY AND CONCLUSION
The study was done on 500 patients admitted to the Neurology department of Sohag university hospital, Alhelal hospital and Sohag general hospital presented by stroke within the first 48 hours. Patients with a history of renal disease or receiving dialysis for chronic renal failure were excluded. Patients were subjected to detailed medical and neurological evaluation. Stroke severity assessed by NIHSS, Glasgow coma scale and MRCS of power. CT brain is done for all patients and laboratory studies including serum urea, creatinine, calculated creatinine clearance, uric acid, electrolyte assessment, random blood sugar, liver functions test, coagulation profile, complete blood count and erythrocyte sedimentation rate. Our study found that the prevalence of renal impairment (creatinine> 1.2 mg) in our series 24.4% and its predictors were age, conscious level, presence of speech abnormality, hypertension, hyperuricemia RHD, drug abuse, presence of casts, crystals and albumin in urine analysis, elevated ALT enzyme, leucocytosis and high ESR.
REFERENCES:
- Carter AM, Catto AJ, Mansfield MW, Bamford JM, Grant PJ: Predictive variables for mortality after acute ischemic stroke. Stroke 2007;38:1873–1880.
- Szymon Brzosko, Tomasz Szkolka, Michal Mysliwiec: Kidney Disease Is a Negative Predictor of 30-Day Survival after Acute Ischaemic Stroke . Nephron Clin Pract 2009;112:79–85.
- Hou SH, Cohen JJ. Diagnosis and management of acute renal failure. Acute Care 1985;11:59-84.
- Groeneveld AB, Tran DD, van der Meulen J, Nauta JJ, Thijs LG. Acute renal failure in the medical intensive care unit: predisposing, complicating factors and outcome. Nephron 1991; 59:602-610.
- Brivet FG, Kleinknecht DJ, Loirat P, Landais PJ. Acute renal failure in intensive care units--causes, outcome, and prognostic factors of hospital mortality; a prospective, multicenter study. French Study Group on Acute Renal Failure. Crit Care Med 1996; 24:192-198.
- de Mendonca A, Vincent JL, Suter PM, Moreno R, Dearden NM, Antonelli M, Takala J, Sprung C, Cantraine F. Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score. Intensive Care Med 2000; 26:915-921.
- Metnitz PG, Krenn CG, Steltzer H, Lang T, Ploder J, Lenz K, Le Gall JR, Druml W. Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med 2002; 30:2051-2058.
- Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Ronco C. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 2005; 294:813-818.
- George Tsagalis, Theodore Akrivos, Maria Alevizaki, Efstathios Manios, Kimon Stamatellopoulos, Antonis Laggouranis and Konstantinos N. Vemmos: Renal dysfunction in acute stroke: an independent predictor of long-term all combined vascular events and overall mortality. Nephrol Dial Transplant 2009;24:194-200.
- Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, the ADQI workgroup. Acute renal failure – definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 2004; 8:204-212.
- Finney H, Newman DJ, Price CP. Adult reference ranges for serum cystatin C, creatinine and predicted creatinine clearance. Ann Clin Biochem 2000;37:49-59.
- Annika Åhlström, Docent VILLE PETTILÄ, MINNA TALLGREN: Acute renal failure in critically ill patients with special reference to prediction of outcome. Helsinki 2006, http://ethesis.helsinki.fi
- Zilong Hao, Bo Wu, Sen Lin, Fan-Yi Kong, Wen-Dan Tao, De-Ren Wang, Ming Liu. Association between Renal Function and Clinical Outcome in Patients with Acute Stroke . Eur Neurol 2010;63:237–242.
- MacWalter RS, Wong SYS, Wong KYK, Stewart G, Fraser CG, Fraser HW, Ersoy Y, Ogston SA, Chen R. Does Renal Dysfunction Predict Mortality After Acute Stroke? A 7-Year Follow-Up Study. Stroke 2002;33:1630-1635.
- Adrian Covic, Adalbert Schiller, Nicoleta-Genoveva Mardare, Ligia Petrica, Maxim Petrica, Adelina Mihaescu and Norica Posta: The impact of acute kidney injury on short-term survival in an Eastern European population with stroke . Nephrol Dial Transplant 2008;23:2228–2234.
- Angela M Carter, Andrew J, Michael W, John M, Peter J. Predictive Variables for Mortality After Acute Ischemic Stroke. Stroke. 2007;38:1873-1880.
- Xue JL, Daniels F, StarRAet al. Incidence andmortality of acute renal failure in Medicare beneficiaries, 1992 to 2001. J Am Soc Nephrol 2006; 17: 1135–1142.