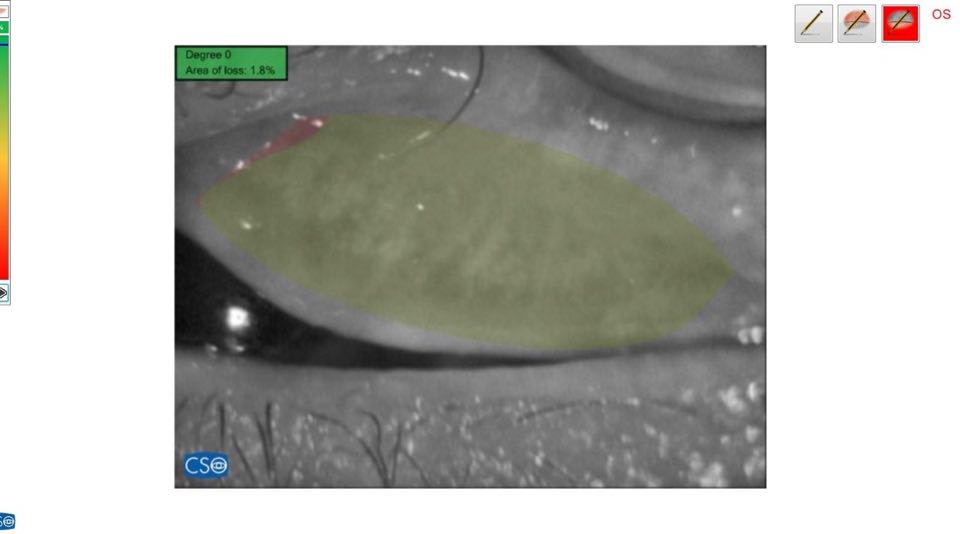
Purpose. To examine the morphological changes in the meibomian glands of patients with keratoconus as well as to study the relationship between these changes in the morphology and several tear film parameters. Methods. Examination of the meibomian gland (MG) of 300 keratoconus patients presenting to the center using infrared noncontact meibography system (Sirius, CSO, Italy) between January 2017—January 2019. 100 eyes of healthy individuals were also enrolled as a control group. Tear breakup time (TBUT) test and Schirmer test II were evaluated. Subjective symptoms were also assessed using Ocular Surface Disease Index (OSDI). Results. Mean age of keratoconus patients was 19 ± 12 years and 21 ± 14 years in control group. Average TBUT was 4.9 ± 2.1 sec. and average Schirmer test was 5.3 ± 2.2 mm which was significantly lower than control group (). Meibomian gland dropout in the lower eyelid of the keratoconus group was as follows: grade 0 (no loss of meibomian glands): 100 eyes; grade 1 (gland dropout area <1/3 of the total meibomian glands): 85 eyes; grade 2 (gland dropout area 1/3 to 2/3): 68 eyes; and grade 3 (gland dropout >2/3): 47 eyes. Conclusion. Keratoconus shows significant meibomian gland dropout and distortion that can be recorded by noncontact meibography. Sirius meibography is a simple, cost-effective method of evaluating meibomian gland dropout as a part of the routine refractive examination.