Mediastinal Tumor
?What are mediastinal tumors
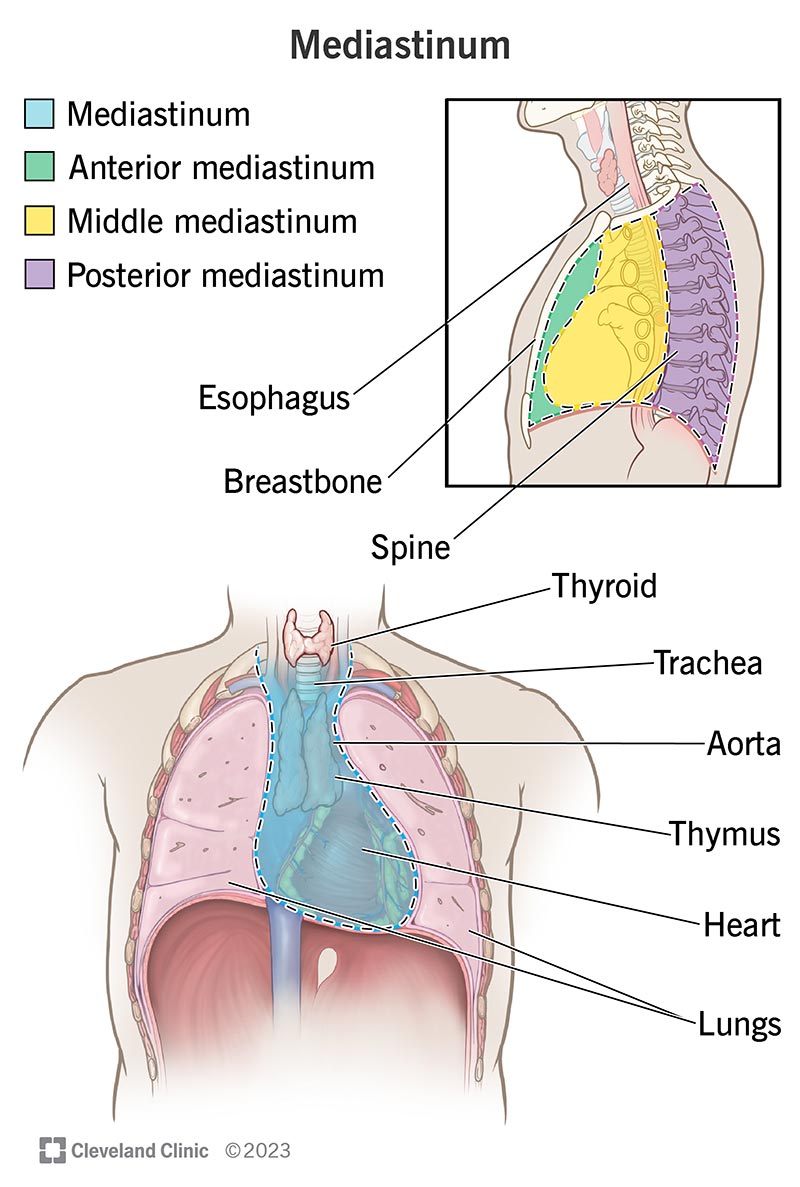
Mediastinal tumors are benign or cancerous growths that form in the area of the chest that separates the lungs. This area, called the mediastinum, is surrounded by the breastbone in front, the spine in back, and the lungs on each side. The mediastinum contains the heart, aorta, esophagus, thymus and trachea.
- The anterior
- The middle
- The posterior
Mediastinum tumors are mostly made of reproductive (germ) cells or develop in thymic, neurogenic (nerve), lymphatic or mesenchymal (soft) tissue
?Who is affected by mediastinal tumors
In general, mediastinal tumors are rare. Mediastinal tumors are usually diagnosed in patients aged 30 to 50 years, but they can develop at any age and form from any tissue that exists in or passes through the chest cavity.
The location of tumors within the mediastinum varies according to the age of the patient. In children, tumors are commonly found in the posterior (back) mediastinum. These mediastinal tumors often begin in the nerves and are typically benign (noncancerous).
In adults, most mediastinal tumors occur in the anterior (front) mediastinum and are generally malignant (cancerous) lymphomas or thymomas.
?Is a mediastinal tumor serious
Due to their location in the mediastinum, mediastinal tumors (both benign and malignant) that are left untreated can cause serious complications including invading the heart, pericardium (the lining around the heart), and great vessels (the aorta and vena cava). Tumors located in the posterior (back) mediastinum can cause compression of the spinal cord.
?What causes mediastinal tumors
There are several types of mediastinal tumors, with their causes linked to where they form in the mediastinum.
Anterior (front) mediastinum
- Germ cell - The majority of germ cell neoplasms (60 to 70%) are benign and are found in both males and females.
- Lymphoma – Malignant tumors that include both Hodgkin’s disease and non Hodgkin’s lymphoma.
- Thymoma and thymic cyst - The most common cause of a thymic mass, the majority of thymomas are benign lesions that are contained within a fibrous capsule. However, about 30% of these may be more aggressive and become invasive through the fibrous capsule.
- Thyroid mass mediastinal – Usually a benign growth, such as a goiter, these can occasionally be cancerous.
Middle mediastinum
- Bronchogenic cyst – A benign growth with respiratory origins.
- Lymphadenopathy mediastinal – An enlargement of the lymph nodes.
- Pericardial cyst – A benign growth that results from an "out-pouching" of the pericardium (the heart’s lining).
- Thyroid mass mediastinal – Usually a benign growth, such as a goiter. These types of tumors can occasionally be cancerous.
- Tracheal tumors – These include tracheal neoplasms and non-euplastic masses, such as tracheobronchopathia osteochondroplastica (benign tumors).
- Vascular abnormalities including aortic aneurysm and aortic dissection.
Posterior (back) mediastinum
- Extramedullary haematopoiesis – A rare cause of masses that form from bone marrow expansion and are associated with severe anemia.
- Lymphadenopathy mediastinal – An enlargement of the lymph nodes.
- Neuroenteric cyst mediastinal – A rare growth, which involves both neural and gastrointestinal elements.
- Neurogenic neoplasm mediastinal – The most common cause of posterior mediastinal tumors, these are classified as nerve sheath neoplasms, ganglion cell neoplasms, and paraganglionic cell neoplasms. Approximately 70% of neurogenic neoplasms are benign. Oesophageal abnormalities including achalasia oesophageal, oesophageal neoplasm and hiatal hernia. Paravertebral abnormalities including infectious, malignant and traumatic abnormalities of the thoracic spine. Thyroid mass mediastinal – Usually a benign growth, such as a goiter, which can occasionally be cancerous. Vascular abnormalities – Includes aortic aneurysms.
?What are the symptoms of a mediastinal tumor
Almost 40% of people who have mediastinal tumors experience no symptoms. Most of the growths are often discovered on a chest x-ray that is performed for another reason. When symptoms are present they are often a result of the compression of surrounding structures, such as the spinal cord, heart or the pericardium (the heart’s lining), and may include:
- Cough
- Shortness of breath
- Chest pain
- Fever
- Chills
- Night sweats
- Coughing up blood
- Hoarseness
- Unexplained weight loss
- Lymphadenopathy (swollen or tender lymph nodes)
- Wheezing
- Stridor (a high-pitched, noisy respiration, which can be a sign of respiratory obstruction, especially in the trachea or larynx)
?How is a mediastinal tumor diagnosed
The tests most commonly used to diagnose and evaluate a mediastinal tumor include:
- Chest x-ray
- Computed tomography (CT) scan of the chest or CT-guided needle biopsy
- Magnetic resonance imaging (MRI) of the chest
- Mediastinoscopy with biopsy (Performed under general anesthesia, this examination of the chest cavity uses a lighted tube inserted through a small incision under the chest bone; a sample of tissue is taken to determine if cancer is present. Mediastinoscopy with biopsy allows doctors to accurately diagnose 80 to 90% of mediastinal tumors, and 95 to 100% of anterior mediastinal tumors.)
?How are mediastinal tumors treated
The treatment used for mediastinal tumors depends on the type of tumor and its location:
- Thymic cancers require surgery, followed by radiation or chemotherapy. Types of surgery include thoracoscopy (a minimally invasive approach), mediastinoscopy (minimally invasive) and thoracotomy (a procedure performed through an incision in the chest).
- Lymphomas are recommended to be treated with chemotherapy followed by radiation.
- Neurogenic tumors found in the posterior (back) mediastinum are treated surgically.
What are the benefits of minimally invasive surgery to treat mediastinal tumors
As compared with traditional surgery, patients who undergo minimally invasive surgery, such as video-assisted thoracoscopy (VATS) mediastinoscopy, experience:
- Decreased postoperative pain
- Shorter hospital stay
- More rapid recovery and return to work
Other possible benefits include reduced risk of infection and less bleeding.
What are the risks of minimally invasive surgery to treat mediastinal tumors
There are complications of radiation, chemotherapy and surgical treatment of mediastinal tumors. Your health care team will discuss the possible risks and potential benefits of each treatment option with you.
The possible complications of minimally invasive surgical treatment include:
- Damage to the surrounding area, which may include the heart, pericardium (the heart’s lining) or spinal cord. Pleural effusion (a collection of fluid between the thin layers of tissue lining the lung and the wall of the chest cavity, or pleura)
- Postoperative drainage
- Postoperative infection or bleeding
Your health care team will provide specific instructions to prepare you for each treatment or procedure. They will also provide specific instructions for your recovery and return to work, including guidelines for activity, driving, incision care and diet.
References
Trupiano JK, Rice TW, Herzog K, Barr FG, Shipley J, Fisher C, and Goldblum JR. Mediastinal synovial sarcoma: report of two cases with molecular genetic analysis, Ann. Thorac. Surg. 2002; 73: 628-630.
Rice et al. Superficial adenocarcinoma of the esophagus, J Thorac Cardiovasc Surg.2001; 122: 1077-1090
Strollo DC, Rosado de Christenson ML and Jett JR. Primary mediastinal tumors. Part 1: tumors of the anterior mediastinum, Chest 1997; Vol 112, 511-522.
GOOD LUCK
Dr. Essam Elbadry
.jpeg)
