Background:
The paraspinal posterior approach to the lumbar spine initially was described for spinal fusion, particularly for the treatment of lumbosacral spondylolisthesis. Wiltse described his approach for lower lumbar and sacral vertebrae by bilateral incisions 4.5 cm lateral to the mid-line going through the natural cleavage plane between the multifidus part of sacrospinalis and the longissimus part. This will carry minimal postoperative back pain with low risk of infection.
Purpose:
We aim in this study to evaluate the modification of the Wiltse approach with its minimal intraoperative blood loss and minimal post-operative complication to be the approach of choice in the management of single level lumbar spine degenerative diseases.
Study design:
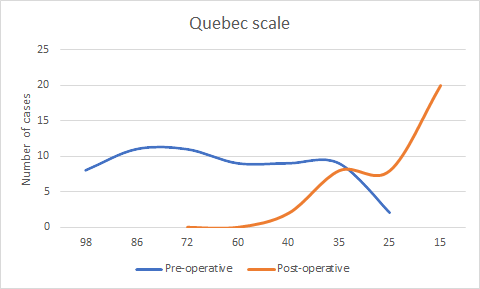
A retrospective study was done in the neurosurgical department at Sohag university hospital on 30 patients between January 2016 and January 2018. Visual analogue scale (VAS) and Quebec disability scale used for post-operative evaluation.
In this study a modification to this approach by single midline skin incision from 3- 5 cm with paraspinal dissection in the same plane described by Wiltse to get access to the transverse process and facet joints with minimal soft tissue dissection and retraction. This is less vascular than the mid-line approach, resulting in less bleeding and less post-operative back pain.
Methods:
Thirty patients with different lumber spine pathologies were operated via modified Wiltse approach by single midline skin incision from 3- 5 cm with paraspinal dissection in the natural plane of the sacrospinalis muscle between the longissimus and multifidus to get access to the transverse process and facet joints with minimal soft tissue dissection and retraction. Unilateral or bilateral facetectomy was done to achieve a good posterior decompression with transpedicular screws and interbody fusion. Patients were followed by complete pre and post-operative neurological assessment. Early and late postoperative complications were recorded. Radiographic follow-up for evaluation of fusion, and evaluating the operative results using both Visual analogue scale (VAS) and Quebec disability scale were done.
Results:
Males were more predominant in this study (60%) with average age 35.36±5.96 years back pain was the most frequent complain (100%) followed by sciatic pain (56%). Pars defect was presented in 17 cases (56.6%). L5-S1 affection was in (63.3%). The low back pain was improved after surgery in all cases. Post-operative hospital stay was average two days. One case presented by postoperative infection (3.3%). Dural tear with postoperative CSF leak was noticed in one patient. Neither complications related to the interbody cage nor screws were observed.
Conclusion:
Mini -open transforaminal lumbar interbody fusion approach provides a low- risk surgery, less intraoperative blood loss, and rapid postoperative recovery with favorable outcome in the management of single -level lumbar spine degenerative diseases.