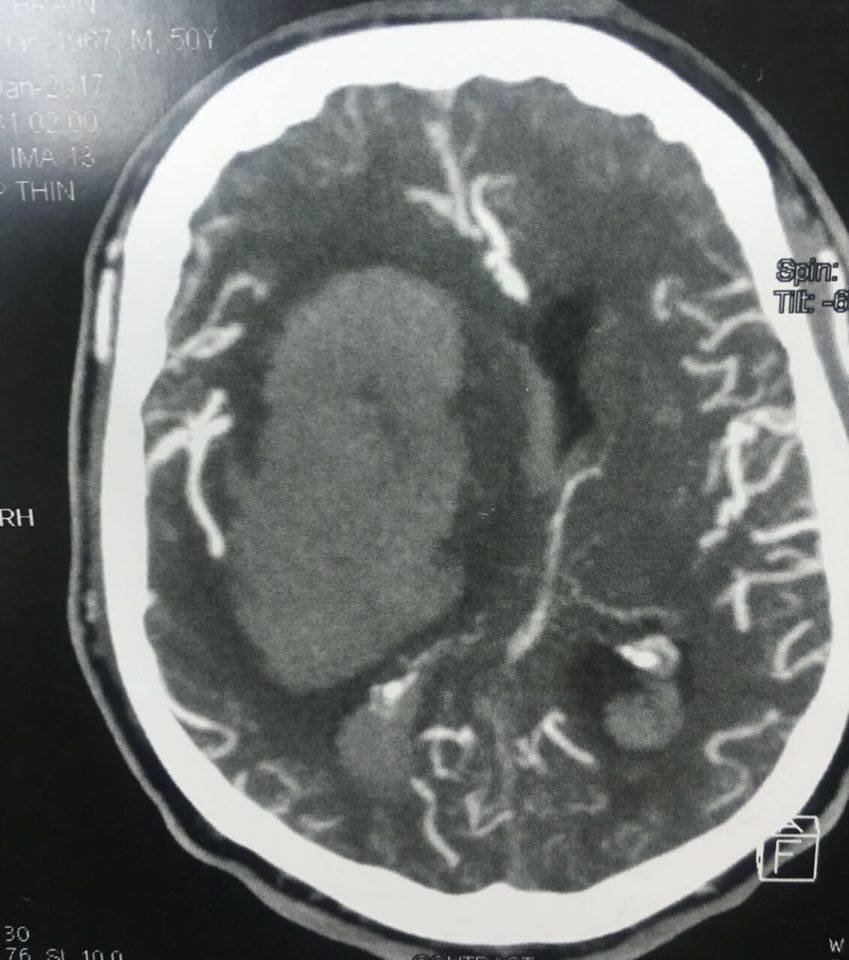
Introduction: Spontaneous intracerebral hemorrhage is a major health problem worldwide; representing 25% of stroke cases. Risk factors include old age, hypertension, amyloid angiopathy, history of anticoagulant intake and cardiovascular disease. The surgical role remains controversial in the literature and this debate is because of the possible brain injury occurring during the evacuation. However, the surgical evacuation may relieve local ischemia and compression caused by the hemorrhage. The aim of the study: To evaluate the surgical evacuation of the spontaneous intracerebral hemorrhage and to detect factors associated with the best prognosis. Patients and method: A prospective case series of 52 patients, who developed spontaneous intracerebral hemorrhage aged 2 months to 55 years, underwent surgical evacuation in the period between November 2012 and October 2015. They were evaluated regarding the degree of hematoma evacuation using postoperative brain CT, and then followed for six months for the functional outcome using modified Rankin score, Glasgow outcome score and mortality rate 3 months postoperatively. Results: The mean age was 31.3 ± 20.4 years. The commonest presentation was disturbed conscious level, repeated convulsions and a neurological deficit. After the surgical evacuation; the survived patients were 28 (53.8%) after 3 months. Thirteen of them (25%) had postoperative morbidity in the form of mono-paresis or hemiparesis. Survival was associated with many factors as a right sided hematoma, early intervention, the volume of hemorrhage and preoperative Glasgow Coma Scale < 8. Conclusion: Spontaneous intracerebral hemorrhage in children is mostly due to coagulopathies while in adults, caused mainly by hypertension. Large intracerebral hematoma, low GCS at the time of presentation and late surgical evacuation worsen patients’ outcome. Better prognosis was associated with the complete evacuation. Meticulous observation of the patients is mandatory as they have a higher incidence of deterioration rapidly.