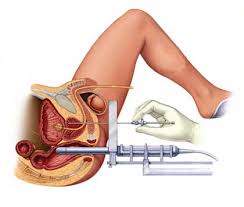
Purpose. – For patients with good urinary function and presenting with a low risk prostate cancer, prostate
brachytherapy using iodine implants represents one of the techniques of reference. This retrospective
analysis investigates urinary (U), digestive (D) and sexual (S) toxicities and their prognostic factors of
duration.
Material and methods. – From August 2000 to November 2007, 176 patients presenting with prostate
adenocarcinoma underwent interstitial brachytherapy. Urinary, digestive and sexual toxicities were classified
according to Common toxicities criteria for adverse events, version 3.0 (CTCAE V3.0). For each
toxicity (U, D, S), the number of complications U (dysuria, nicturia. . .), D (proctitis, diarrhea. . .) and S
(sexual dysfunction, loss of libido, . . .) was listed and analyzed according to criteria related to the patient,
implant, dosimetric data and characteristics of the toxicity. Prognostic factors identified in univariate
analysis (UVA) (Log Rank) were further analyzed in multivariate analysis (MVA) (Cox model).
Results. – With a median follow-up of 26 months (1–87), 147 patients (83.5 %) presented urinary toxicities.
Among them, 29.5 % (86 patients) and 2.4 % (seven patients) presented grade 2 and 3U toxicity
respectively. In UVA, urinary grade toxicity greater than or equal to 2 (p = 0.037), the presence of initial U
symptoms (p = 0.027) and more than two urinary toxicities (p = 0.00032) were recognized as prognostic
factors. The number of U toxicities was the only prognostic factor in MVA (p = 0.04). D toxicity accounted
for 40.6 % (71 patients). Among them, 3 % (six patients) were grade 2. None were grade 3. Two factors were
identified as prognostic factors either in UVA and MVA: the number ofDtoxicities greater than or equal to
2 (univariate analysis: p = 0,00129, multivariate analysis: p = 0,002) and age less than or equal to 65 years
(univariate analysis: p = 0,004, multivariate analysis: p = 0,007). Eighty-three patients (47.4 %) presented
a sexual toxicity; 26.9 % (49 patients) and 5 % (nine patients) were scored as grade 2 and 3 respectively.
A number of seeds greater than 75 (p = 0.032) and S grade greater than or equal to 2 (p < 0.0001) were
recognized as prognostic factors in UVA. S grade was the only prognostic factor in MVA (p = 0.0015).
Conclusion. – The duration of U, D and S toxicity is strongly correlated with a high number of toxicities
and the grade of toxicity. This analysis allows for better information given to the patient regarding the
duration of the post-treatment complications.