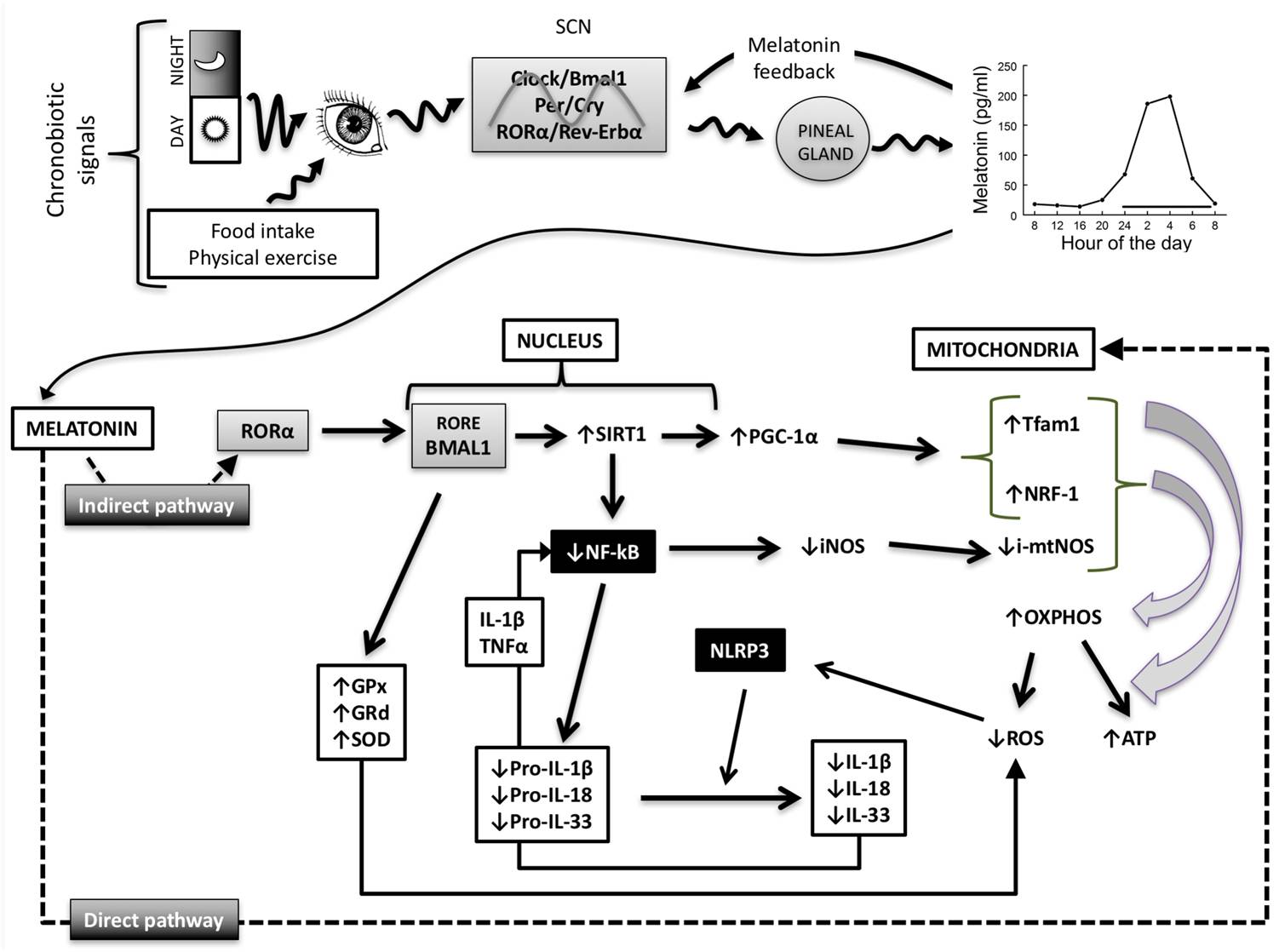
After the characterization of the central pacemaker
in the suprachiasmatic nucleus, the expression of
clock genes was identified in several peripheral tissues
including the immune system. The hierarchical control from
the central clock to peripheral clocks extends to other functions
including endocrine, metabolic, immune, and mitochondrial
responses. Increasing evidence links the disruption
of the clock genes expression with multiple diseases and
aging. Chronodisruption is associated with alterations of the
immune system, immunosenescence, impairment of energy
metabolism, and reduction of pineal and extrapineal melatonin
production. Regarding sepsis, a condition coursing
with an exaggerated response of innate immunity, experimental
and clinical data showed an alteration of circadian
rhythms that reflects the loss of the normal oscillation of
the clock. Moreover, recent data point to that some mediators
of the immune system affects the normal function of the clock. Under specific conditions, this control disappears
reactivating the immune response. So, it seems that clock
gene disruption favors the innate immune response, which
in turn induces the expression of proinflammatory mediators,
causing a further alteration of the clock. Here, the clock
control of the mitochondrial function turns off, leading to a
bioenergetic decay and formation of reactive oxygen species
that, in turn, activate the inflammasome. This arm of
the innate immunity is responsible for the huge increase of
interleukin-1β and entrance into a vicious cycle that could
lead to the death of the patient. The broken clock is recovered
by melatonin administration, that is accompanied by
the normalization of the innate immunity and mitochondrial
homeostasis. Thus, this review emphasizes the connection
between clock genes, innate immunity and mitochondria
in health and sepsis, and the role of melatonin to maintain
clock homeostasis