Objective Cost-effectiveness analysis is an approach used to determine the value of a medical care option and refers to a method used to assess the costs and health benefits of an intervention. Upon the diagnosis of liver cirrhosis, the current guidelines recommend that all cirrhotic patients have to be screened for the presence of esophageal varices by endoscopy. In addition, patients with a positive family
history of esophageal cancer are screened annually. These approaches place a heavy burden on endoscopy units, and repeated testing over time may have a detrimental effect on patient compliance
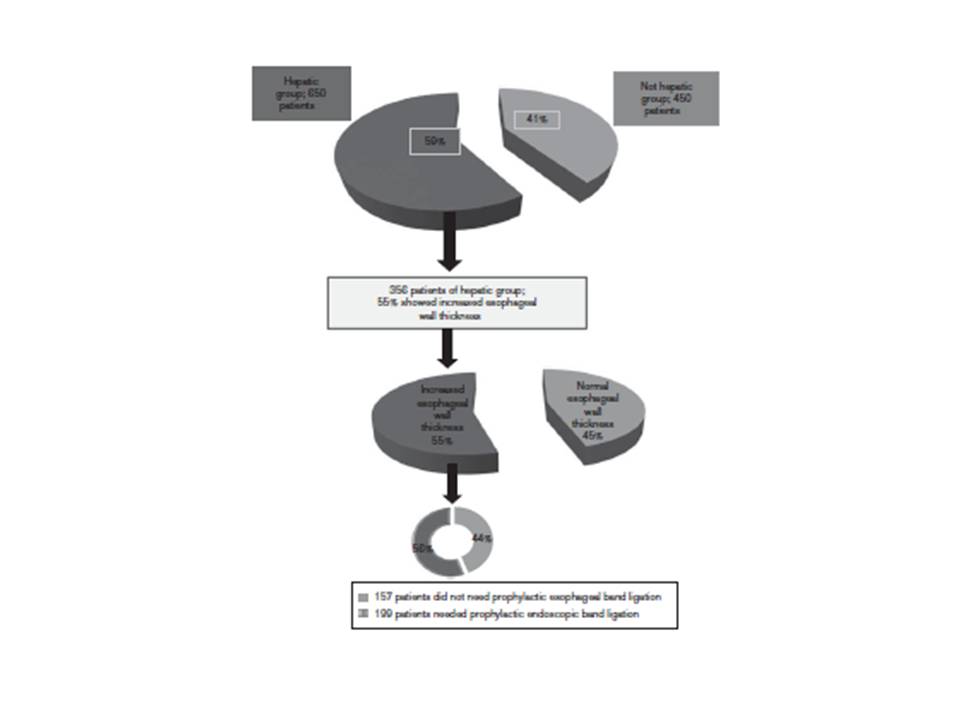
Patients and methods Following the recommendations of a recent study entitled ‘Detection of risky esophageal varices using two dimensional ultrasound: when to perform endoscopy’, the intra-abdominal portion of the esophagus of 1100 patients was divided into a hepatic group, which included 650 patients, and a nonhepatic group, which included 450 patients, who presented with manifestations of liver
diseases and gastrointestinal symptoms, respectively, and were examined using standard two-dimensional ultrasound (US) to evaluate cost effectiveness, standard issues, and medical benefits using conventional US.
Results The overall effectiveness analysis of 1100 patients yielded a 41% cost standard benefit calculated to be $114 760 in a 6-month study.
Conclusion Two-dimensional US can play an important role in screening for esophageal abnormalities, thus saving money and time. The esophagus should be screened during routine conventional abdominal US.