| Anatomy |
- Biomechanics
- weight bearing leads to net compressive forces on medial cortex and tensile forces on lateral cortex
|
| Classification |
| |
| Russel-Taylor Classification |
| Type I |
No extension into piriformis fossa |
  |
| Type II |
Extension into greater trochanter with involvement of piriformis fossa
• look on lateral xray to identify piriformis fossa extension |
  |
• Historically used to differentiate between fractures that would amenable to an intramedullary nail (type I) and those that required some form of a lateral fixed angle device (type II)
• Current interlocking options with both trochanteric and piriformis entry nails allow for treatment of type II fractures with intramedullary implants |
|
| |
| AO/OTA Classification Examples |
| 32-A3.1 |
Simple (A), Transverse (3), Subtrochanteric fracture (0.1) |
 |
| 32-B3.1 |
Wedge (B), Fragmented (3), Subtrochanteric fracture (0.1) |
 |
| 32-C1.1 |
Complex (C), Spiral (1), Subtrochanteric fracture (0.1) |
 |
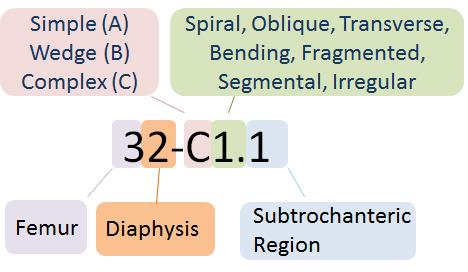 Facture Location Facture Location 
• Femur (3) , Diaphysis (2), Subtrochanteric region (0.1)
Fracture Pattern
• Simple (A), Wedge (B), Complex (C)
|
|
| |
|
ASBMR Task Force Case Definition of Atypical Femur Fractures (AFFs), Revised criteria
Four of five major features should be present to designate a fracture as atypical; minor features may or may not be present in individual cases
|
| Major Criteria |
- Associated with no trauma or minimal trauma, as in a fall from a standing height or less
- Fracture originates at the lateral cortex and is substantially transverse in its orientation, although it may become oblique as it crosses the medial femur
- Noncomminuted
- Complete fractures extend through both cortices and may be associated with a medial spike; incomplete fractures involve only the lateral cortex
- Localized periosteal or endosteal thickening of the lateral cortex is present at the fracture site
|
| Minor Criteria |
- Generalized increase in cortical thickness of the femoral diaphyses
- Prodromal symptoms such as dull or aching pain in the groin or thigh
- Bilateral incomplete or complete femoral diaphysis fractures
- Delayed fracture healing
- Specifically excluded are fractures of the femoral neck, intertrochanteric fractures with spiral subtrochanteric extension, pathological fractures associated with primary or metastatic bone tumors, and periprosthetic fractures
|
|
| |
| Presentation |
- History
- long history of bisphosphonate or denosumab
- history of thigh pain before trauma occurred
- Symptoms
- hip and thigh pain
- inability to bear weight
- Physical exam
- pain with motion
- typically associated with obvious deformity (shortening and varus alignment)
- flexion of proximal fragment may threaten overlying skin
|
| Imaging |
- Radiographs
- recommended views
- AP and lateral of the hip
- AP pelvis
- full length femur films including the knee
- optional views
- traction views may assist with defining fragments in comminuted patterns but is not required
- findings
- proximal fragment flexed and abducted

- distal fragment adducted and ER

- bisphosphonate-related fractures have

- lateral cortical thickening
- increased diaphyseal cortical thickness
- transverse vs. short oblique fracture orientation
- medial spike (if complete fracture)
- lack of comminution
|
| Treatment |
- Nonoperative
- observation with pain management
- indications
- non-ambulatory patients with medical co-morbidities that would not allow them to tolerate surgery
- limited role due to strong muscular forces displacing fracture and inability to mobilize patients without surgical intervention
- Operative
- intramedullary nailing (usually cephalomedullary)

- indications
- historically Russel-Taylor type I fractures
- newer design of intramedullary nails has expanded indications
- most subtrochanteric fractures treated with IM nail

- fixed angle plate
- indications
- surgeon preference
- associated femoral neck fracture
- narrow medullary canal
- pre-existing femoral shaft deformity
|
| Techniques |
- Intramedullary Nailing
- position
- lateral positioning

- advantages
- allows for easier reduction of the distal fragment to the flexed proximal fragment

- allows for easier access to entry portal, especially for piriformis nail
- supine positioning
- advantages
- protective to the injured spine
- address other injuries in polytrauma patients
- easier to assess rotation
- techniques
- 1st generation nail (rarely used)
- 2nd generation reconstruction nail
- cephalomedullary nail
- trochanteric or piriformis entry portal
- piriformis nail may mitigate risk of iatrogenic malreduction from proximal valgus bend of trochanteric entry nail
 
- pros
- preserves vascularity
- load-sharing implant
- stronger construct in unstable fracture patterns
- cons
- reduction technically difficult
- nail can not be used to aid reduction
- fracture must be reduced prior to and during passage of nail
- may require percutaneous reduction aids or open clamp placement to achieve and maintain reduction
 
- mismatch of the radius of curvature
- nails with a larger radius of curvature (straighter) can lead to perforation of the anterior cortex of the distal femur

- complications
- varus malreduction (see complications below)
- Fixed angle plate
- approach
 
- lateral approach to proximal femur

- may split or elevate vastus lateralis off later intermuscular septum
- dangers include perforating branches of profunda femoris
- technique
- 95 degree blade plate or condylar screw
- sliding hip screw is contraindicated due to high rate of malunion and failure
- blade plate may function as a tension band construct

- femur eccentrically loaded with tensile force on the lateral cortex converted to compressive force on medial cortex
- cons
- compromise vascularity of fragments
- inferior strength in unstable fracture patterns
|
| Complications |
- Varus/ procurvatum malunion

- the most frequent intraoperative complication with antegrade nailing of a subtrochanteric femur fracture is varus and procurvatum (or flexion) malreduction
- Nonunion

- can be treated with plating
- allows correction of varus malalignment
- Bisphosphonate fractures

- nail fixation
- increased risk of iatrogenic fracture
- because of brittle bone and cortical thickening
- increased risk of nonunion with nail fixation resulting in increased need for revision surgery
- plate fixation
- increased risk of plate hardware failure
- because of varus collapse and dependence on intramembranous healing inhibited by bisphosphonates
|