Summary
Prognosis of patients with early inflammatory arthritis (EIA) is highly variable.
The aim of this study was to compare, longitudinally and crosssectionally,
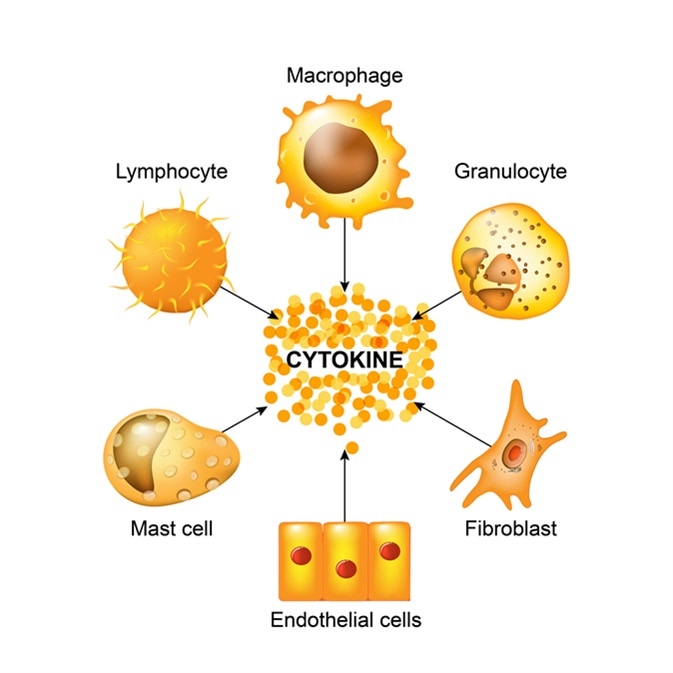
the levels of cytokine-expressing cells in peripheral blood (PB)
from patients with EIA to those in established rheumatoid arthritis (RA) and
healthy controls (HC). PB mononuclear cells from HC (n = 30), patients with
EIA (n = 20) or RA (n = 38) were stimulated with phorbol myristate acetate
(PMA)/ionomycin for 3 h, and stained for cell markers and cytokines. Serum
cytokines and chemokines were measured by Luminex. Patients with EIA
were reassessed at 6 and 12 months. The percentage of interleukin (IL)-
17+interferon (IFN)-γ−CD4+ T cells [T helper type 17 (Th17)] was increased
in RA and EIA versus HC. Serum IL-1β, IL-2, IL-4 IL-17 and macrophage
inflammatory protein (MIP)-1α were increased in RA and EIA versus HC.
IL-1Ra, IL-15 and IFN-α were increased in EIA versus HC. IL-6 and tumour
necrosis factor (TNF)-α was increased in RA but not EIA versus HC. Disease
activity scores in EIA patients improved over 12 months’ treatment. Th17
percentage at baseline was correlated with both rheumatoid factor (RF) titre
and functional deficit at 12 months. Baseline levels of serum granulocyte–
macrophage colony-stimulating factor (GM-CSF), IL-6 and IL-8 were correlated
with Larsen score at 12 months. There were no significant changes in
cytokine-expressing CD4+T cells over time, although the percentage of IL-6+
monocytes increased. IL-17+CD4+ T cells and serum IL-17 levels are
increased in EIA. IL-6-expressing monocytes increase during the first year of
disease, irrespective of disease-modifying anti-rheumatic drug (DMARD)
therapy. We observed incomplete clinical responses, suggesting EIA patients
need more intensive early therapy.