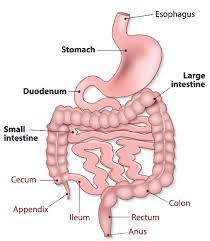
Gastrointestinal involvement (GI) in systemic sclerosis (SSc) is one of the most frequent symptoms in SSc and include a wide range of symptoms from gastro-oesophageal reflux to faecal incontinence. These have a negative impact on patient quality of life. The SSc_GIT 1.0 is a disease-specific HRQOL instrument for patients with SSc to assess their GIT-related activity and severity, High-resolution manometry (HRM ) enables a detailed assessment of esophageal pressure characteristics and makes it possible to study the interaction between pressure in the stomach, lower esophageal pressure (LES), upper esophageal pressure (UES), and esophageal body in detail.
We studied the relation between the SSc_GIT 1.0 and the HRM findings in scleroderma patients,
Methods: Forty systemic sclerosis (SSc) patients were diagnosed according to 1980 ACR classification criteria, recruited during their routine monthly follow-up. Patients answered the UCLA SCTC GIT1.0 irrespective of whether they had a history of GI symptoms. HRM was done in 24 patients at the same visit as the GIT1.0
Results: 32 female and 8 male patients, with mean disease duration 9.3 years, mean age 46 years, 31 patients had dcSSc, and 9 patients had LcSSc, Average (SD) of GIT 1.0 score was 0.95±0.62. 85.7% of patients reported upper and 75% lower GI symptoms, while 5% of patients reported no symptoms. The GIT 1.0 was categorized as 0 - “None- - Mild”( score 0.00-0.49), “Moderate”(score 0.5-1.0) and “Severe-to- Very severe”(score: 1.01-3.0) based on the designations of the scores in the questionnaire. For the total GI symptoms 45% had severe to very severe symptoms, 25% were moderate, while 30% had non to mild symptoms.
HRM findings were classified into two groups (normal and abnormal); the abnormal group represents patients with low esophageal sphincters pressure with or without peristalsis. HRM abnormality was associated with worse: total GIT (p<0.003), reflux (p<0.01), distension (p<0.01) and emotional (p<0.005) scores.
Discussion: These data show that the GIT1.0 reflects UGI function, thus potentially enhancing the usefulness of the GIT1.0. Although the GIT1.0 was never validated with respect to separate domains, these data imply that this possibility exists. Although scoring domains separately was not initially tested, this potential deserves and requires more validation and research.
Conclusion: HRM correlates with SSc GIT1.0 questionnaires, especially with some upper GI domains (reflux, distension), emotional effects and overall score.